Transplantation & Cellular Therapy
The latest news, research, and perspectives in transplantation and cellular therapy. Autologous and allogeneic hematopoietic stem cell transplantation represent potentially curative options for some patients, while the field of non-transplant cellular therapies, such as chimeric antigen receptor (CAR) T-cell therapies, CAR natural killer cell therapies, and genetically modified T-cell receptors, is also expanding to offer more patients curative options.
Advertisement
Advertisement
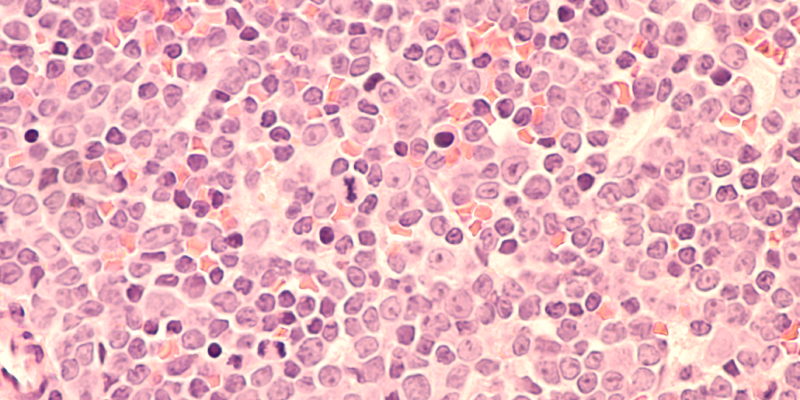
In approximately 12,000 reports of adverse events, the researchers found 19 cases of T-cell malignancies after CAR-T.
The investigators reviewed case reports of patients 20 years old and younger who underwent therapy for BPDCN.
HMA plus venetoclax was found to be effective and well tolerated in patients with AML who relapsed after HSCT.
Adding ofatumumab to reduced intensity conditioning is safe and effective in high-risk B-cell non-Hodgkin lymphoma.
The study also explored the role of this combination in transitioning patients to HSCT.
The award grants $100,000 to a postdoctoral or early-career oncology researcher from a racial/ethnic minority group.
The multicenter, single-arm phase II trial evaluated axicabtagene ciloleucel in patients with MZL or follicular lymphoma.
Nicolaus Kröger, MD, discusses a study on GVHD and its impact on relapse in patients with myelofibrosis undergoing HSCT.
Drs. Dahiya and Spiegel return for the second half of a discussion on reports of secondary T-cell malignancies after CAR-T.
Approach-oriented coping was associated with higher quality of life and lower symptoms of depression and anxiety.
The study used public data from various online sources related to approved CAR-T therapies for MM.
The mandate could affect moving CAR-T therapies into earlier lines of therapy for multiple myeloma.
This manufacturing process change results in a shorter manufacturing time for axi-cel from 16 days to 14 days.
ZUMA-7 showed that axi-cel significantly improved OS compared with standard of care in relapsed or refractory LBCL.
The latest HemOnc Pulse episode looks at the science behind the statement from the FDA on the risk of CAR-T therapies.
Patients' coping strategies prior to HSCT had significant effects on their psychological distress and quality of life.
Shernan Holtan, MD, and the hosts discuss recent data on graft versus host disease prophylaxis.
GVHD affects approximately 30,000 Americans, according to Dr. Michael Chancellor, Chief Medical Officer at Lipella.
The investigation is "likely not going to change the risk-benefit profile of these approved products," Dr. Chari said.
Dr. Osman discussed menin inhibitors for leukemia, and axatilimab treatment for graft-versus-host disease.
The analysis included 346 patients with CALR-mutated MF who were transplanted in 123 centers between 2005 and 2019.
Here’s what they add to the treatment toolbox for hematologic malignancies.
In this episode of "The Fellow on Call," the hosts focus on CAR-T, bispecific antibodies, and more.
Dr. de Lima discusses progress and remaining challenges with allogeneic CAR-T and other cellular therapy products.
Ibrutinib has a monthly sticker price of $17,000 and was taken by 20,000 people who were beneficiaries of Medicare.
Critical drugs used to treat cancer are in short supply in the United States and around the globe.
Researchers conducted the study because patients with TP53-mutated disease “have poor outcomes with standard approaches."
CART-ddBCMA is an investigational new drug for the treatment of patients with relapsed or refractory multiple myeloma.
There was a median of two production slots per month from March 2021 to October 2021. All slots were filled.
The difference in infection rates between the treatment and placebo groups was not statistically significant.
Dr. DiPersio discusses events that shaped his career, his lab’s most transformative research, and the future of transplant.
Omidubicel-onlv is a “substantially modified” allogeneic cord blood-based cell therapy.
Dr. June has made “seminal contributions” to CAR T-cell therapy for blood cancers,
Nearly half of caregivers reported a high use of approach-oriented coping strategies.
None of the patients with DDX41 variants who received post-HSCT cyclophosphamide developed severe acute GVHD.
The overall neutrophil response rate, defined as recovery or improvement, was 84% within a median of nine days.
Dr. Pickl discusses potential future uses and implications of a novel biomarker to predict responses to CAR-T in DLBCL.
Dr. Bishop discusses the matter with host Chadi Nabhan, MD, MBA, FACP, and speaks about why CAR-T doesn't always work.
Brexucabtagene autoleucel led to “high rates of durable response” in adults with relapsed/refractory B-cell ALL.
The study's investigators identified a four-gene model that segregated patients with different survival probabilities.
The study used natural language processing for computer-assisted review of electronic health records.
The investigators plan to continue using the monitoring strategies and further study patient outcomes.
The research has implications for patients with hematologic malignancies who need to undergo allogeneic HSCT.
BMS-986393, a GPRC5D-directed CAR-T, had a "favorable” safety profile with “promising” preliminary efficacy in R/R MM.
Survival outcomes are typically poor in patients with relapsed/refractory aggressive BCL who relapse after anti-CD19 CAR-T.
Post-transplant cyclophosphamide]-based GVHD prophylaxis mitigates the development of gastrointestinal GVHD.
Children with R/R B-cell ALL who received co-administered CD19-and CD22-directed CAR-T therapy had a 99% CR.
Allogeneic CAR T-cells had “encouraging safety and efficacy” in patients with CD7-positive hematologic malignancies.
Axicabtagene ciloleucel led to higher response rates and higher toxicity rates than tisagenlecleucel in R/R DLBCL.
Allogeneic off-the-shelf CAR T-cells “showed evidence of antileukemic activity” in heavily pretreated patients...
Blood Cancers Today delivers the latest news, education, and information relevant to hematologic oncology patients and practices.
Sign up to receive Blood Cancers Today eNewsletters: